It took Richard Huckabee 9 years to get a Parkinson’s prognosis.
A district supervisor for a comfort retailer chain, he first observed signs in 2004 when his voice would abruptly falter whereas chatting with massive teams of staff. “It’s most likely simply stress,” Huckabee remembered his physician saying. A yr later got here the mind fuzziness, with Huckabee forgetting his colleagues’ names, having his ideas freeze mid-conversation, and absolutely dropping his capacity to multitask. At this level, his physician satisfied him he had Lyme illness and put him on steroids. “It was terrible. For six months, they mentioned, ‘Simply hold making an attempt,’” Huckabee recounted.
Earlier than the signs began when he was 44, Huckabee was within the prime of his profession, having acquired a promotion and brought over a brand new territory in northern Virginia. “What managers took 80 hours to do, I’d do in 35 hours,” he mentioned proudly. However in 2011, the corporate terminated Huckabee as a result of he was not in a position to do his job. “I couldn’t argue with them as a result of I knew I had points,” Huckabee continued. No physician, nevertheless, may inform him why.
Huckabee’s story is sadly all too widespread. In 2019, 40% of Medicare beneficiaries residing with Parkinson’s, or practically 250,000 People, didn’t see a neurologist for his or her illness, in accordance with a brand new research that’s the largest up to date evaluation of well being care utilization amongst Parkinson’s sufferers. This research, printed Monday in npj Parkinson’s Illness, additionally discovered that 80%-90% of those Medicare sufferers didn’t meet with a bodily, occupational, or speech-language therapist and that over 95% with despair or nervousness didn’t see a psychological well being skilled.
Throughout practically all metrics, these gaps in care have been worse for Asian, Black, Hispanic, and Native People, in addition to girls and rural People. For example, round 5% of Black, Hispanic, and Native American sufferers — and seven.8% of Asian sufferers — noticed a motion issues neurologist, in comparison with about 10% of white sufferers.
The research, funded by the Michael J. Fox Basis and Parkinson’s Basis, drives dwelling the extent to which many Parkinson’s sufferers battle to entry care for his or her bodily and psychological well being. With about one million People residing with Parkinson’s and practically 90,000 new circumstances being recognized every year, the research highlights the necessity for bettering care coordination between major care suppliers and specialists, increasing coaching for basic neurologists, and bettering entry to take care of communities of colour.
What’s driving the gaps in care?
There a number of causes to clarify these disparities, with Parkinson’s sufferers misplaced at each step of the best way, in accordance with a half-dozen geriatricians, neurologists, affected person advocates, and psychological well being professionals interviewed by STAT.
The problem begins with identification of the sickness, as a result of there isn’t a diagnostic take a look at for Parkinson’s or perhaps a customary presentation of illness. “It’s received motor, cognitive, psychiatric, and different bodily signs. It’s not only one illness,” mentioned Laura Marsh, a professor of neurology and psychiatry at Baylor School of Drugs, “after which every of these motor, cognitive, psychiatric points progress in numerous methods.”
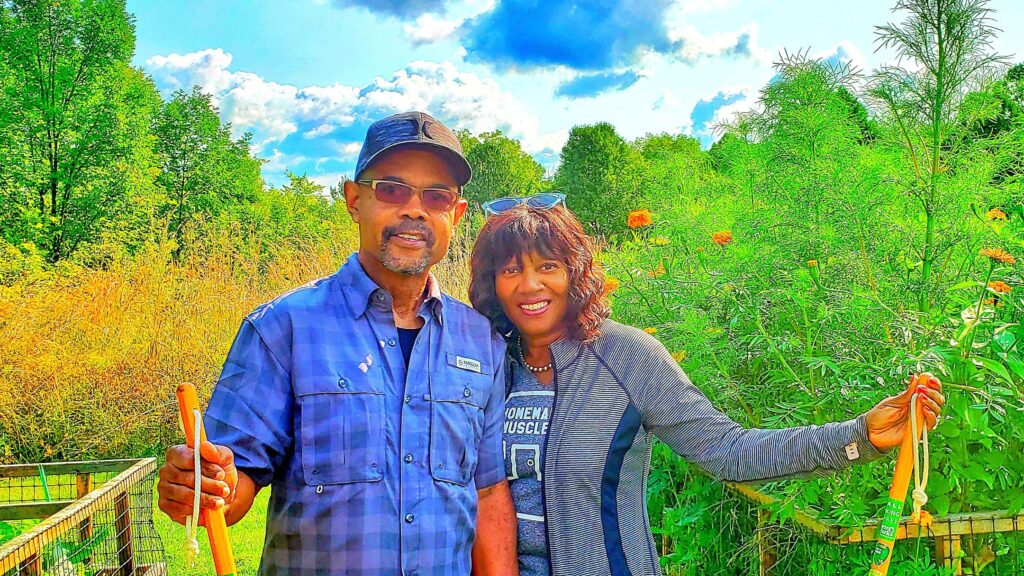
A Black man, Huckabee mentioned his prognosis was additional sophisticated as a result of his signs have been repeatedly dismissed and ignored by his physicians, maybe as a result of 85% to 90% of Parkinson’s sufferers are white. “We don’t match the profile,” Huckabee mentioned. “A number of the docs mentioned I’m taking it too critical,” he added. “A few of them mentioned, ‘There’s nothing flawed with you.’”
In response to Vanderbilt College professor of geriatric medication and senior vp for well being fairness Consuelo Wilkins, tales like Huckabee’s are far too widespread, particularly with important biases in who will get specialty referrals — and, by extension, entry to a prognosis and better ranges of care.
Even a referral is usually not sufficient for some Parkinson’s sufferers as a result of there merely aren’t sufficient neurologists. James Beck, chief scientific officer of the Parkinson’s Basis and senior writer of the brand new research, estimated that, throughout the U.S., there are 3,000 to 4,000 neurologists that see Parkinson’s sufferers and solely 660 movement-disorders neurologists, who’re specifically educated to take care of these sufferers.
On common, that interprets to roughly 1 subspecialist per 1,000 Medicare beneficiaries with Parkinson’s. However these subspecialists are additionally not unfold out uniformly throughout the nation, with solely six working towards in rural areas. Doctor shortages may assist clarify why 30% of sufferers with Parkinson’s had their care managed by a major care supplier and 10% didn’t see any doctor in any respect in 2019.
Past months-long ready lists and difficulties scheduling appointments, some sufferers merely can’t make it or don’t really feel comfy going to their appointments. Certainly, Wilkins famous that neurologists and movement-disorder specialists are predominantly situated in suburban white neighborhoods, making it harder for communities of colour to entry their providers. “If English will not be your most well-liked or major language, then who’s there and out there to supply that care — culturally and linguistically applicable?” Wilkins requested. “The disparities and inequities simply begin to compound.”
The research’s psychological well being findings are additionally notably disappointing, in accordance with Roseanne Dobkin, a scientific psychologist and professor of psychiatry at Rutgers College. Within the research, 53% of Parkinson’s sufferers had a prognosis of despair or nervousness, however lower than 2% had a scientific psychologist go to — and fewer than 4% a psychiatry go to.
Psychological well being stigma might assist clarify why these charges are so low, with sufferers afraid to speak about their signs or see a specialist, in accordance with Marsh, the professor at Baylor. So, she thinks a part of the answer could be to broaden the illness narrative.
“Parkinson’s isn’t just a motion dysfunction,” Dobkin equally emphasised. “Despair and nervousness are signs of Parkinson’s illness. They’re not a mirrored image of private failure, or weak spot, or inadequacy.” The truth is, Marsh mentioned that lots of her sufferers have nervousness or temper issues even earlier than they discover out they’ve Parkinson’s.
The stakes are excessive for getting these sufferers entry to psychological well being care, with despair cascading into sooner charges of bodily and cognitive decline, larger charges of caregiver misery, and elevated charges of well being care utilization and prices, Dobkin mentioned. “All of us must spend extra time specializing in and speaking in regards to the neuropsychiatric points of the illness course of, identical to specialists spend large time speaking in regards to the motor points.”
Want for elementary adjustments
Sharon Brangman, chief of geriatrics at SUNY Upstate Medical College, mentioned she acknowledges the worth of quantifying these gaps in Parkinson’s care. “However I’m undecided what number of extra wants assessments we’d like,” Brangman mentioned. “What’s wanted are elementary adjustments, and that’s the place the onerous work comes.”
Maria Moro-de-Casillas, a motion issues neurologist at Hartford HealthCare, is aware of this intimately nicely. After noticing for years that Hispanic sufferers have been underrepresented and receiving lower-quality care within the hospital’s Parkinson’s clinic, she opened the Spanish-Language Motion Dysfunction Clinic in 2020 to sort out three key boundaries: transportation, language, and tradition. For one, the clinic was intentionally arrange in downtown Hartford to be extra central and accessible by public transport. Secondly, there are not any translators on this clinic. “All of the individuals who work with me are both Hispanic themselves or well-versed in Hispanic tradition,” mentioned Moro-de-Casillas.
That cultural sensitivity is the essential third part as a result of “the kind of care that you simply present in your common suburban clinic,” she mentioned, “will not be going to work in a minority clinic.” For instance, recognizing the basic unit of household in Hispanic tradition, she invitations sufferers’ kids and grandchildren to the appointments. And understanding how troublesome it’s to brazenly discuss psychological well being, she proactively explains to sufferers that despair and nervousness are regular signs and nothing to be ashamed about.
“I feel the Lord despatched her to me,” mentioned 73-year-old Luis Muniz, who confessed to Moro-de-Casillas that he was feeling depressed after his spouse died. “She’s coping with my actions, however she is so useful and type. She offers with my different issues as nicely,” from levels of cholesterol to sleep high quality to reminiscence loss.
Different teams have taken an identical method to offering culturally competent Parkinson’s care, from Tufts College researchers working a scientific trial on creating extra inclusive applications for Asian People to College of Arizona clinicians internet hosting neurology clinics at Indian Well being Service and tribal well being care services on the Navajo and Hopi reservations.
The Veterans Well being Administration might provide one other template for addressing therapy gaps for Parkinson’s sufferers, regardless of shortages in specialists. Within the VA, a nurse follows up with sufferers to trace psychological well being signs over time, and in the event that they don’t enhance, the first care physician consults a psychiatrist, in accordance with Marsh, who can be the manager director of the Psychological Well being Care Line on the Michael E. DeBakey VA Medical Middle. With psychiatrists targeted on seeing sufferers with probably the most extreme circumstances which may not be responding to therapy and supporting major care physicians in any other case, a small group of psychological well being professionals can take care of a a lot bigger group of sufferers.
The VA has an identical system for neurology care as nicely, that includes a hub-and-spoke mannequin with six specialised Parkinson’s facilities throughout the nation and dozens of regional specialty clinics to supply care nearer to dwelling. In coordinating care and sharing experience, a restricted variety of motion issues specialists can thus take care of a better affected person inhabitants.
‘Felt like a merciless joke’
When Huckabee was lastly recognized with Parkinson’s by a neurologist, he was each elated and crushed. “I used to be glad to seek out out what I lastly had,” mentioned Huckabee. “I used to be devastated at 9 years of in-and-out docs, and right here is that this one physician that claims in 10 minutes, ‘You’ve got Parkinson’s illness.’” It felt like a merciless joke.
Now on the Cleveland Clinic, Huckabee has a complete workforce managing his care, from a motion issues neurologist who enrolled him in new analysis trials to an occupational therapist who helped him learn to drive once more. Just a few years in the past, Huckabee even began seeing a therapist after a drug he was prescribed led to a playing dependancy. “It received so unhealthy that my spouse was nearly prepared to go away me,” Huckabee mentioned. However his therapist was in a position to rehabilitate that relationship and, in session together with his neurologist, get him off that treatment.
Huckabee acknowledges that he simply occurred to be fortunate — fortunate to reside close to a world-class tutorial medical heart, fortunate to have a Medicare plan that covers all his Parkinson’s care, and fortunate to lastly be recognized. “We want extra specialised locations so that individuals of colour may really feel extra comfy, may really feel just like the docs actually care,” mentioned Huckabee.