In Brazil, a gaggle of researchers has reported the most important outbreak thus far of COVID-associated candidemia brought on by the identical drug-resistant pressure of Candida parapsilosis, a fungus that invades the bloodstream and might result in loss of life. The outbreak occurred in 2020-21 in an intensive care unit (ICU) at a tertiary referral hospital in Salvador, Bahia state, throughout one of many peaks of the COVID-19 pandemic.
In an article printed within the journal Rising Microbes and Infections, the researchers warn of the chance that different drug-resistant strains will emerge in future and stress the significance of practices that assist keep away from fungal infections in hospitals.
“We carried out a research through which we analyzed blood samples from extreme COVID-19 sufferers on the hospital and located that 90% of these contaminated by this species of Candida had strains proof against or tolerant of fluconazole and echinocandins, the 2 most important lessons of antifungals used to deal with invasive candidiasis. Virtually 60% of those sufferers died,” mentioned Arnaldo Colombo, a professor on the Federal College of São Paulo’s Medical Faculty (EPM-UNIFESP) and principal investigator for the research.
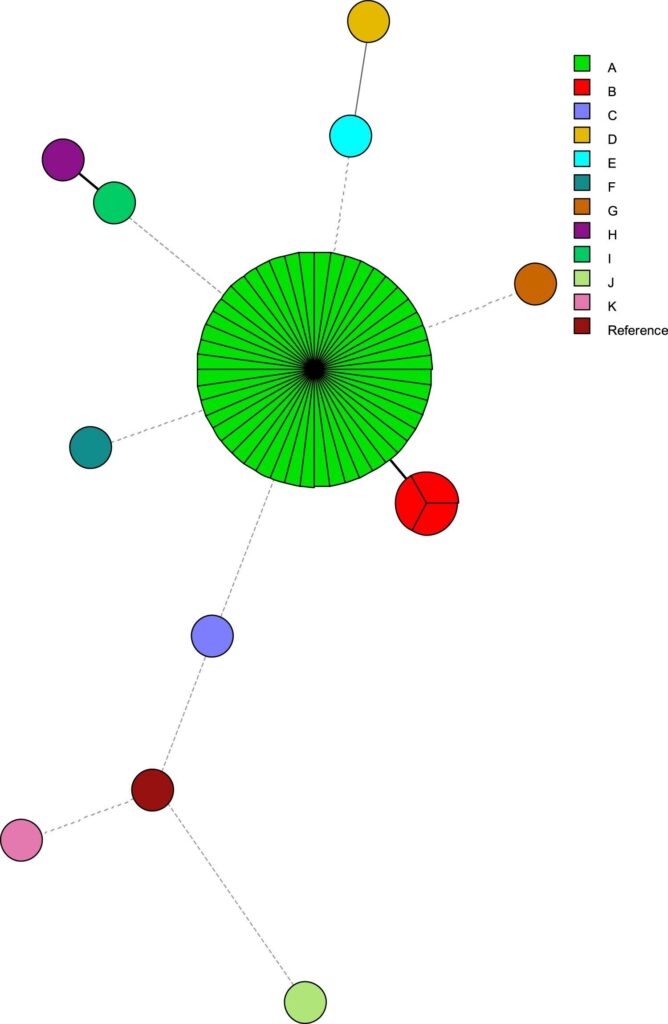
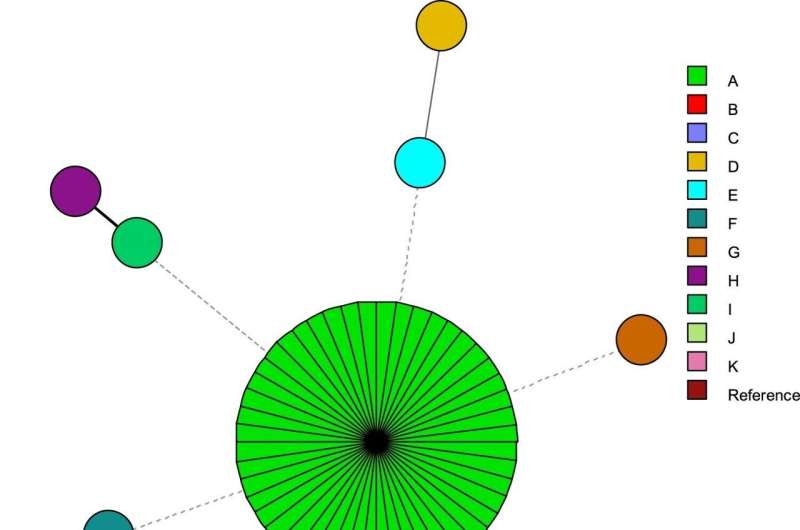
The researchers analyzed 60 isolates cultured from 57 sufferers who had developed C. parapsilosis candidemia within the hospital’s COVID-19 ICU. Genetic typing confirmed that 51 (85%) of the fluconazole-resistant isolates belonged to the identical cluster (had the identical widespread ancestor), whereas the inclined isolates every represented a definite lineage. A part of them had been additionally echinocandin-tolerant. Echinocandins are used towards fluconazole-resistant strains of Candida.
Drug resistance might be outlined as the event by a microorganism of the power to multiply even within the presence of a drug that often kills it. When an antimicrobial reduces however doesn’t block proliferation, the microorganism is claimed to be tolerant of that drug.
“Circulation of the drug-resistant pressure was most likely facilitated by a well being employee who did not carry out correct hand cleaning and contaminated vascular catheters used to manage drugs and different infusions immediately into the bloodstream. That may occur when ICUs are overcrowded and workers are overworked,” mentioned João Nóbrega de Almeida Júnior, a co-author of the research and a researcher at FM-USP’s basic and instructing hospital.
Pandemic situations
The pressure additionally most likely turned drug-resistant owing to indiscriminate use of antifungals in treating high-risk sufferers with lengthy hospital stays. The follow is widespread in sufferers with extreme illness who stay unstable.
“Assessments to detect microorganisms take time and in emergency conditions physicians might use antibiotics and antifungals empirically, focusing on the most probably brokers of an infection. Ideally, therapy of sepsis [generalized infection] ought to entail the focusing on of a number of completely different microorganisms, however the follow needs to be rationalized to forestall the event of resistance, toxicity and extra prices,” mentioned Colombo, who can be a researcher and infectious illness specialist at Hospital São Paulo, UNIFESP’s instructing hospital.
In Brazil, most well being facilities lack the wherewithal to conduct checks of susceptibility to antifungals, hindering early recognition of drug-resistant strains. This drawback facilitates the unfold of fungal infections within the healthcare system.
Equally, if an agent just isn’t characterised earlier than an an infection is handled, the affected person could also be given an ineffective drug. On this context, the researchers harassed the significance of correct analysis earlier than antifungals are administered, in addition to the necessity for complete molecular testing to characterize resistant brokers.
The research confirmed that mutations within the gene ERG11, usually thought of an indicator of resistance to the category of antifungals that features fluconazole, had been current in solely 35.8% of the samples. Then again, all resistant samples had a mutation in TAC1, which elevated expression of CDR1, a gene accountable for efflux pumps, a resistance mechanism whereby resistant fungal strains purchase the power to pump the drug out of their cells, decreasing its focus and therapeutic potential.
When this genetic mutation emerged in strains of C. parapsilosis that had been initially delicate to fluconazole, doses of the medicine needed to be elevated eightfold as a way to begin inhibiting their progress. Different mutations had been discovered within the gene FKS1, in a area the place alterations of the type are unusual.
“They’re tolerant of the drug. Killing them requires greater doses. This implies we might quickly discover strains which can be proof against this class of drug, which is presently prescribed for fluconazole-resistant fungi,” Almeida Júnior warned.
Selection
In gentle of their evaluation of this outbreak, the researchers stress the significance of conducting checks for fungal drug resistance in medical facilities and advocate the usage of liposomal amphotericin B to fight drug-resistant Candida, though it may have opposed negative effects and prices greater than fluconazole or echinocandins.
“We have to set up decision-making algorithms and biomarkers in order to make use of antibiotics and antifungals sparingly and with the appropriate doses and timing. That will keep away from the emergence of resistant strains,” mentioned Colombo, who’s working with ANVISA, the Brazilian well being surveillance authority, on protocols for therapy of fungal infections by the SUS, the nationwide well being service.
Indiscriminate use of antibiotics can be a threat issue for fungal an infection, he added. They kill intestine microorganisms and might make the partitions of the intestines extra permeable, letting into the bloodstream fungi of the genus Candida that stay within the human intestine however don’t trigger illness underneath regular situations.
Systemic Candida infections happen above all within the hospital surroundings, the place there are immunocompromised sufferers and invasive procedures reminiscent of hemodialysis, mechanical air flow and intravenous drug administration can let Candida into the bloodstream.
Among the many sufferers within the research pattern, 54% had been utilizing a catheter when the an infection was identified. The general 30-day mortality charge was 59.6%.
Farnaz Daneshnia et al, Determinants of fluconazole resistance and echinocandin tolerance in C. parapsilosis isolates inflicting a big clonal candidemia outbreak amongst COVID-19 sufferers in a Brazilian ICU, Rising Microbes & Infections (2022). DOI: 10.1080/22221751.2022.2117093
Quotation:
Submit-pandemic outbreak of drug-resistant fungus in Brazil stemming from abuse of medicines and full ICUs (2022, November 30)
retrieved 1 December 2022
from https://medicalxpress.com/information/2022-11-post-pandemic-outbreak-drug-resistant-fungus-brazil.html
This doc is topic to copyright. Aside from any truthful dealing for the aim of personal research or analysis, no
half could also be reproduced with out the written permission. The content material is supplied for info functions solely.