Even as the US has made commitments to well being as a human proper and reversing well being disparities and has invested considerably in orphan ailments, it continues to miss sickle cell illness (SCD), the commonest inherited blood dysfunction worldwide, which impacts greater than 100,000 People, most of whom are Black or Hispanic American.
As hematologists who care for folks with sickle cell illness, it’s disheartening to see this situation obtain solely a fraction of the eye and assets that different inherited issues obtain. Cystic fibrosis, for instance, which impacts roughly 30,000 People, receives 10 occasions the federal funding.
The disparities don’t cease there. Individuals with sickle cell illness typically aren’t believed once they describe their ache, with some being falsely labeled as drug seekers. Others have restricted entry to specialists due to their insurance coverage.
commercial
Altering this troubling establishment would require altering the present, reactionary method to managing sufferers with sickle cell illness to embody all facets of their well being. We imagine the important first step is for Congress to move the Sickle Cell Illness Complete Care Act (S. 3389 and H.R. 6216). It could set up federal funding for state Medicaid applications to create particular facilities to supply complete, preventive outpatient look after folks with sickle cell illness with a deal with younger adults and pregnant folks.
Sickle cell illness happens in folks with two atypical copies of the gene for “sickle” beta hemoglobin. This gene happens primarily in descendants of individuals from areas the place malaria is prevalent akin to sub-Saharan Africa, Southeast Asia, and Central America. It’s because having a single copy of this gene, which causes what’s often called sickle cell trait, ends in decrease oxygen focus within the pink blood cells, limiting the expansion of the parasite that causes malaria, however doesn’t trigger vital sickling of pink blood cells.
commercial
In conditions of stress or low oxygen, the pink blood cells of individuals with sickle cell illness can grow to be “C”-shaped, just like the farm device often called a sickle. These cells don’t reside so long as regular pink blood cells, and so they can get caught inside small blood vessels. This could trigger fixed, typically debilitating ache and multi-organ issues, together with strokes, blood clots, kidney failure, liver failure, and early demise — the common lifespan of ladies within the U.S. with sickle cell illness is 43 years, and 41 years for males.
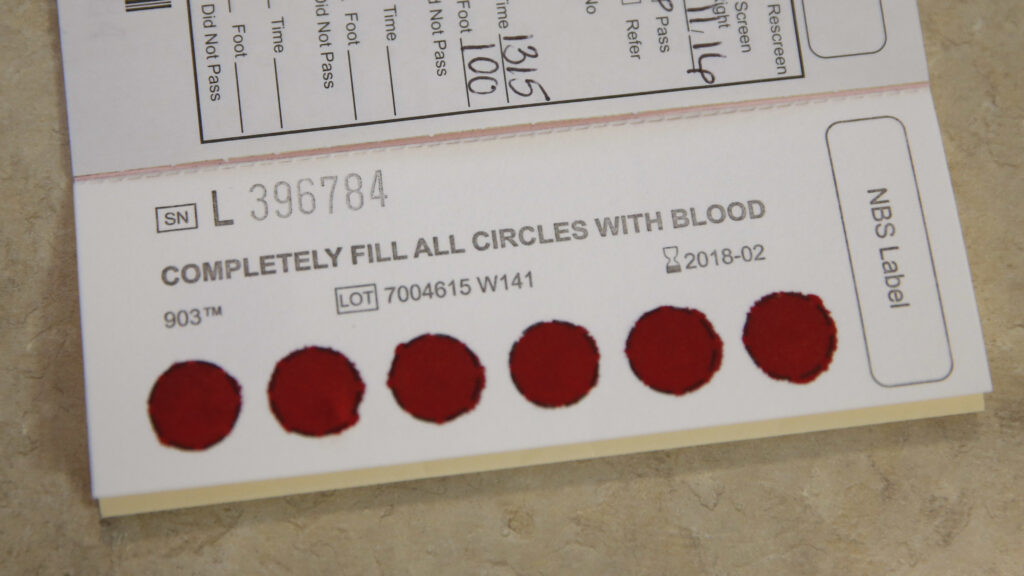
Although all newborns within the U.S. are presupposed to be examined for sickle cell illness, there isn’t any system to make sure all that each one infants recognized as having it are referred to a specialist. There may be additionally little data out there on the place most individuals with sickle cell illness reside or how they entry the well being system.
Preliminary efforts to enhance the understanding of SCD epidemiology embody the passage of laws just like the Sickle Cell Illness and Different Heritable Blood Problems Analysis, Surveillance, Prevention, and Remedy Act of 2018, which has offered funding to the Facilities for Illness Management and Prevention to start sickle cell illness surveillance and registry-building applications in 11 states. The early returns on funding have been vital, notably in California and Georgia, the place these information have been used to direct assets to areas beforehand missing specialised look after sickle cell illness. This program must be expanded to different states.
For greater than 70 years after sickle cell illness was found, there have been no medication to deal with this dysfunction. The primary, hydroxyurea, grew to become out there within the Eighties. Up to now few years, advances in analysis on sickle cell illness are being translated to therapies, leading to three new FDA-approved drugs, enhancements in healing stem cell transplants, and transformative gene therapies that would probably change how we deal with sickle cell illness.
But entry to those therapies has remained restricted, as not all people with sickle cell illness can entry the specialists who can present them. That is partly as a result of considerably fewer folks with sickle cell illness who’re lined by applications like Medicaid are seen by hematologists (7%) than these lined by industrial insurance coverage (43%) — and the next proportion of individuals with sickle cell illness are lined by Medicare and Medicaid (roughly 60%) than these with different inherited hematologic circumstances (20% to 40%). Entry is additional restricted by a paucity of hematologists with specialty coaching or data of sickle cell illness, and the restricted reimbursement for the therapy they supply and the complexity of care required for folks with this illness.
Caring for people with sickle cell illness is exceedingly costly, with an estimated lifetime value of $1.7 million per particular person — which is probably going an underestimate. This is because of excessive prices of care delivered within the emergency division, primarily for extreme ache crises when an elevated quantity of the sickled pink blood cells out of the blue clump in small blood vessels, the restricted entry to sickle cell specialists, and the multi-organ dysfunction ensuing from this illness. Constant preventive administration is required to interrupt this vicious cycle of emergency division and hospital admissions and readmissions, however the U.S. well being care system, particularly for folks lined by Medicaid, will not be at present constructed to reward preventive or complete care. Funding in these providers, nevertheless, has actual potential for general financial savings.
For significant progress to be made, the U.S. must fund complete care facilities for sickle cell illness, related in design to the nation’s almost 150 complete hemophilia therapy facilities that features provisions for psychological well being in addition to crucial eye and dental care. The Nationwide Alliance for Sickle Cell Facilities was based to acknowledge sickle cell facilities, however there isn’t any federal funding to help their upkeep or the mandatory high quality enchancment actions wanted to enhance therapy. These facilities might be supported by way of the Middle for Medicare and Medicaid Innovation or, ideally, by way of the Sickle Cell Illness Complete Care Act, which has lively bipartisan help. This funding construction would permit for extra of those therapy facilities to type and develop, whereas placing techniques in place to make sure high-quality look after folks with SCD.
These complete facilities can be hubs of specialists skilled to handle the complete spectrum of sickle cell illness, with the first goals being to forestall among the illness’s most excessive penalties and to extend the size and high quality of life. With higher continuity of care, folks with the illness may obtain personalised care plans to handle routine issues and thereby keep away from pointless visits to emergency departments. Offering acceptable care that stops debilitating issues would permit affected people extra freedom to interact in gainful employment. These facilities may additionally implement improvements akin to day hospitals to supply blood transfusions, intravenous fluids, and ache drugs with out emergency division visits. Day hospitals and specialised infusion facilities have demonstrated value financial savings and improved care high quality, but lower than half of the acknowledged sickle cell facilities have day hospitals on account of restricted funding.
These facilities may grow to be financially self-sustaining if the care they supply is appropriately reimbursed, whereas on the identical time realizing the underlying objectives of improved high quality of care and correction of structural inequities. This may symbolize a measurable dedication to enhancing the standard and entry to look after folks with SCD.
To make certain, these options alone received’t repair generations of underlying problems with systemic and overt racism which have resulted in disbelief of particular person’s descriptions of their SCD-related ache and routine undertreatment. For a program of complete facilities to efficiently enhance entry to symptomatic and preventive care, it would should be accepted by the sickle cell group, since generations of mistreatment have contributed to a scarcity of religion — if not outright mistrust — within the well being system.
To reverse generations of injustice to the sickle cell group, a considerable funding in public funds is required for information assortment and dissemination of assets, training and coaching, formation of particular complete care facilities, and monetary and social help for sufferers to entry these providers. Reaching all of this requires complete care plan for folks with sickle cell illness.
Amar Kelkar is a hematologist on the Dana-Farber Most cancers Institute in Boston and an teacher in medication at Harvard Medical College. Julie Kanter is a hematologist, director of the Grownup Sickle Cell Illness Program, and an affiliate professor of hematology and oncology within the Division of Hematology and Oncology on the College of Alabama at Birmingham. Payal Desai is a hematologist, director of the Sickle Cell Illness Enterprise, and an affiliate professor on the Levine Most cancers Institute at Atrium Well being in Charlotte, N.C.
First Opinion publication: In case you take pleasure in studying opinion and perspective essays, get a roundup of every week’s First Opinions delivered to your inbox each Sunday. Join right here.